Doctors and nurses who performed the surgery immediately after it was completed. The first successful uterus transplant took place in Great Britain. The patient’s older sister was the donor. Both women are doing well. The surgery itself took place over a week ago, but it was only reported now that the sisters had avoided potential complications that could have been very serious.
According to the surgeons, both were “on cloud nine” after the successful double operation, which will allow the younger sister to have children. The operation took over nine hours at the Oxford hospital. Both women asked that their names not be used. The older sister is 40 years old, has two children, and has decided not to have any more. Her younger sister was born with Mayer-Rokitansky-Küster-Hauser syndrome (MRKH), a rare developmental disorder in which girls are born with an underdeveloped vagina and an underdeveloped or absent uterus. The first symptom of the disorder is the absence of menstruation in adolescent girls. It affects approximately one in 5000 women worldwide.
In addition, the ovaries of women with this syndrome are not damaged and function normally, so the only obstacle to childbirth is the absence of a uterus. Previously, these patients could only have biological children through surrogacy. The success of the transplants means that they are now able to carry their own children, although natural childbirth remains inaccessible to them and babies are born by cesarean section.

Uterus transplantation is different from other organ transplants in that it is not done for life, but for a few years to allow a woman to give birth. After that, the organ is removed and the woman can lead a normal life without taking immunosuppressive drugs.
“We explain quickly, simply and clearly what happened, why it matters and what will happen next.” The number of offers should remain: episodes. End of Story Podcast Advertising
Prior to surgery, the younger sister underwent two cycles of ovulation stimulation to retrieve eggs that were fertilized with her husband’s sperm to create embryos. Five of the most viable embryos were frozen to be transplanted into a donor uterus in the event of a successful transplant. Currently, the transplanted uterus is functioning exactly as it should, according to lead surgeon Professor Smith. If the embryo transfer into the uterus is successful, the woman will need to take immunosuppressants throughout the pregnancy to prevent rejection of the donor organ. However, unlike a heart or liver transplant, a uterus transplant is limited in time. Doctors expect that after approximately five years and one or two successful pregnancies, the uterus will be removed and immunosuppressants will no longer be necessary.
The second uterus transplant is scheduled to be performed on another woman in the UK this fall, and several other patients are waiting for their turn.

Isabel Kiorga (left) and Richard Smith (right) during surgery.
The primary responsibility for the operation fell on the shoulders of two surgeons: Professor Richard Smith of Imperial College London and Isabelle Kirogi of the Oxford Transplant Centre. The first part of the operation was to remove the uterus from the recipient’s 40-year-old sister. It took eight hours and twelve minutes. The surgeons were careful not to touch the ovaries so as not to induce early menopause in the woman.
They began surgery on the younger sister about an hour earlier, preparing her body to receive a donor organ. The operation lasted nine hours and 20 minutes. According to available reports, the doctors encountered some difficulties, especially with the higher than expected blood loss, which amounted to two liters (the total amount of blood in a person’s body is about five liters).
In addition to being a consultant gynecologist, Professor Smith is the clinical director of the charity Womb Transplant UK. According to him, the technique of this operation is similar to a radical hysterectomy (removal of the uterus). Surgeons removed the older sister’s uterus along with the fallopian tubes and major blood vessels surrounding the organ.
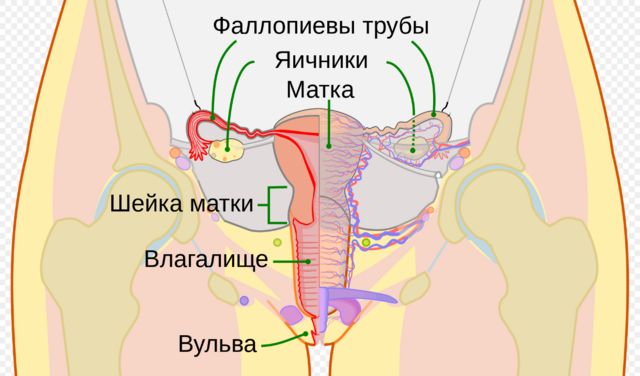
Surgeons had to remove the donor’s uterus without damaging the ovaries and preserving the blood vessels. “One of the most interesting moments is that, as Professor Smith said, as an oncology surgeon, I am used to removing organs while “sealing” the blood vessels. Whereas in transplantation it is necessary to take a normal organ [from the donor’s body] with as many ‘unsealed’ blood vessels as possible.”
Smith and Kiroga worked together from the beginning, extracting the uterus from the eldest sister’s body and then moving it from the donor to the recipient. The professor noted that even the first step was not easy because the donor’s uterus had an unusual blood supply. “There were a number of blood vessels that I had never seen before in my life. So it was very difficult to remove the organ, but we did it,” he added.
The most important part of the transplant was the connection of very small vessels that supply blood to the uterus, which was performed by Isabelle Kiroga. At the same time, the main difficulties with uterine transplantation usually occur immediately after the operation, and their probability is 20 to 25%. Smith noted that surgeons have long been technically ready to perform such surgeries, but currently the likelihood of failure is high. The chances of an unfavorable outcome decrease after three to four days, and already two weeks after a woman receives a uterus and experiences her first menstrual period, the chances of her being able to give birth to a child are very high, and the chances of serious complications decrease to a minimum.

Isabelle Kiroga and Richard Smith.
According to Smith, neither tried to pull the ceiling toward them. Both surgeons moved around the operating table to where they were most needed. When uterus transplantation becomes routine, women born with MRKH syndrome will have the opportunity to carry a child into the world. Until now, their hopes for motherhood have been limited to either adoption or surrogacy. Surrogacy is legal in the UK, but there are many legal complications. For example, the court cannot force the biological parents to fulfill the surrogacy contract regarding the transfer of the child. The surrogate becomes the official mother of the child at birth, and if she has a husband or partner, he is considered the official father of the child until he relinquishes his parental rights.
Despite the fact that uterine transplantation seems to be a desirable prospect, such operations currently require the fulfillment of a number of conditions, not only medical ones. For example, both sisters were interviewed by a psychologist to confirm their ability to cope with any potential consequences. And the operation itself was pre-approved by the UK’s Human Tissue Authority (HTA), which regulates the legal aspects of the removal, storage, use and disposal of human bodies, organs and tissues.
According to the professor, “the shocking truth is that currently in the country more than 15 thousand women of childbearing age suffer from uterine infertility. It can be caused either by congenital defects or by the removal of the uterus due to cancerous tumors or other disorders”.

Subscribe to our email newsletter, and every night from Monday through Friday you will receive the most important news of the day, as well as context to help you understand what is happening.
![]()

The British National Health Service is short of both money and hospital beds. In this situation, it is not reasonable to expect them to fund uterus transplants. The world’s first uterus transplant surgery was performed in Sweden in 2014, after which the woman was able to give birth to a child. She received the organ from a friend who was 60 years old at the time. Since then, approximately 100 uterine transplants have been performed worldwide, resulting in the birth of approximately 50 children, primarily in the United States and Sweden, but also in Turkey, India, Brazil, China, the Czech Republic, Germany, and France.
There have been successes, of course, but uterus transplantation is a rare operation that the UK National Health Service does not currently provide free of charge (to the patient). The cost of the operation itself, including the use of medical equipment, drugs and facilities, was £25,000, paid for by the charity Womb Transplant UK, and more than 30 health workers who performed the operation refused to be paid. In total, doctors currently have permission for 15 similar operations for which there are already donors: five living and 10 in a vegetative state, but it will take about £300,000 to carry them out, which will have to be found somewhere.

Lidia Brain hopes that after the uterus transplant, she will be able to give birth to a child. One of the women waiting her turn is 31-year-old Lydia Brain, who had her uterus removed six years ago after being diagnosed with cancer.


